by
Michael Warren, Policy Adviser
| Apr 10, 2018
When we hear the word ‘regulation’ we probably think it is something removed from our daily lives. Or we may think of it as something which stops us from doing something we want to do. It conjures up associations with ‘red tape’, but where would we be without it, especially in the context of health and care?
.png?sfvrsn=d1207320_19) Without even realising it, we come into contact with regulated professionals all the time (solicitors, architects, veterinary nurses to name just a few). When we visit doctors or dentists for our regular check-ups we probably don’t give much thought about who regulates them and makes sure that they continue to be fit to treat us. How many of us are likely to search regulators’ registers to check credentials? (Or even know that there is such a thing as a regulator’s register?) Very few of us probably – unless something goes wrong. We take it for granted that those treating us have the right qualifications.
Without even realising it, we come into contact with regulated professionals all the time (solicitors, architects, veterinary nurses to name just a few). When we visit doctors or dentists for our regular check-ups we probably don’t give much thought about who regulates them and makes sure that they continue to be fit to treat us. How many of us are likely to search regulators’ registers to check credentials? (Or even know that there is such a thing as a regulator’s register?) Very few of us probably – unless something goes wrong. We take it for granted that those treating us have the right qualifications.
However, if we do decide to delve deeper into the regulation of healthcare professionals in the UK, we might find it difficult to navigate our way through this complex system. We are not alone. Soon after becoming US president, Donald Trump remarked, ‘Nobody knew healthcare could be so complicated.’ Healthcare systems across the world are complicated, and healthcare regulation in the UK is no different.
This two-part blog will explore and explain one small part of the UK healthcare system: the regulation of professionals (or ‘professional regulation’). We’ll provide an overview on how many practitioners are regulated, who regulates them and some of the differences between those regulators. Part two of this blog will discuss some of the challenges regulators are facing as well as look at alternatives to statutory regulation.
What is professional regulation?
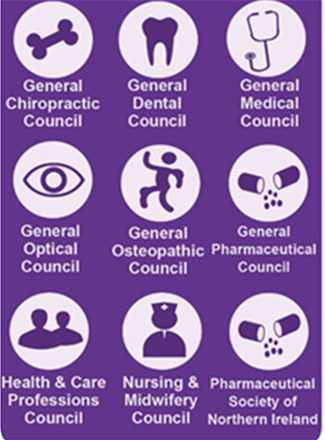
Ask yourself: how do I know my doctor is up-to-date with all the latest developments in medicine? Who makes sure that the optician carrying out my eyesight tests knows what they are doing? Who sets the standards and codes of practice that healthcare professionals need to follow? The answer: the 10 statutory UK health and care regulators.
Regulation is simply a way to make sure that healthcare professionals are safe to practise and remain safe to practise throughout their career, but it is far from simple itself. It is designed to protect us by limiting the risks we may face when receiving treatment. In UK healthcare, regulation does not just apply to people but also touches many areas, from hospitals to equipment to medicines.
There are different ways to ensure that healthcare workers are suitable to provide care. One of these is statutory regulation, often simply referred to as ‘regulation’. This is implemented by the law.
Why do we have regulation?
Regulating health and care professionals is designed to limit the risk of harm occurring to us when we receive treatment or care. Of course, it cannot fully eradicate the risk of harm. The regulators have one main objective and that is to protect the public. This can be broken down into three broad goals:
- protecting the public
- maintaining public confidence in the profession and/or
- declaring and upholding professional standards.
Of the three goals, the second is arguably the most elusive. The public is a large and diverse group meaning gauging public confidence in a profession can be a tricky task.
A recent example: maintaining public confidence in the profession
This element played a role in the recent high-profile case of Dr Bawa-Garba who has been struck off following a court case in which she was found guilty of gross negligence manslaughter. At a fitness to practise tribunal, she was suspended from practising for 12 months. However, her regulator, the General Medical Council, considered that a decision not to remove Dr Bawa-Garba from practice did not maintain public confidence in the medical profession. They subsequently appealed the tribunal’s ruling in the High Court and Dr Bawa-Garba was removed from the medical register.
Editor's Note: Dr Bawa-Garba was subsequently reinstated to the GMC's register following an appeal.
|
Who is regulated and who decides who is regulated?
Why is a hearing aid dispenser regulated, but an audiologist (hearing therapist) not? Why is an arts therapist regulated, but a play therapist not?
This is not an easy question to answer – professional regulation has evolved over centuries, some regulated professions have grown out of medieval guilds, whereas others have been regulated where a new profession emerges, and a risk associated with it is identified.
However, if you glance at the complete list of regulated professionals you may struggle to see any rhyme or reason behind it. Under current statutory healthcare regulation, there are 32 regulated occupations ranging from doctors, dentists and nurses to pharmacists, opticians and osteopaths. To work in any of these 32 professions, professionals must be registered with the appropriate regulator. The government is responsible for deciding which occupations are regulated.
Who are the regulators and what do they do?
 When you asked: ‘How do I know my doctor is up-to-date with all the latest developments in medicine?’ The answer would be: ‘By checking the General Medical Council’s register’. The regulators have four main functions to ensure that those they register are fit to treat us. They do this by:
When you asked: ‘How do I know my doctor is up-to-date with all the latest developments in medicine?’ The answer would be: ‘By checking the General Medical Council’s register’. The regulators have four main functions to ensure that those they register are fit to treat us. They do this by:
- setting standards of competence and conduct which health and care professionals must meet in order to register and practise, this includes updating and/or producing new guidance (for example, 10 years ago professional behaviour on social media would not have been something regulators would need to cover)
- checking the quality of education and training courses to make sure they give students the skills and knowledge to practise safely and competently
- maintaining a register of professionals which everyone (including the public) can search, but also making sure that the professionals on their registers remain fit to practise. After all a doctor or dentist could pass their exams, start practising and never look at another textbook again. However, regulators are there to make sure that this does not happen. They have various systems in place to gather evidence that their registrants continue to develop professionally and keep up-to-date with developments in their chosen field
- investigate complaints about people on their register and decide if they should be:
- allowed to continue to practise (also known as being fit to practise)
- allowed to continue to practise but with conditions on how they should work (for example, attending a training course)
- suspended from practising
- struck off the register (also known as ‘erasure’), either because of problems with their conduct or their competence.
This process is commonly known as fitness to practise.
In addition to these functions, some regulators will have other responsibilities. For example, the General Pharmaceutical Council also registers and inspects pharmacies.
How similar are the regulators?
There are similarities and differences. As mentioned above they all have the same basic core functions and they are all directly accountable to the Parliaments that hold their legislation. However, the number of registrants each regulator is responsible for varies greatly. For example, the Nursing and Midwifery Council has the largest register with over 690,000 nurses and midwives, whilst the Pharmaceutical Society of Northern Ireland registers 2,470 pharmacists and 548 pharmacies.
Some regulators like the General Chiropractic Council regulate one profession each, whilst the Health and Care Professions Council registers 16 different professions. There are also differences between regulators in their registration fees and fitness to practise processes. Meanwhile, the General Optical Council is the only regulator to register students. These are just a few of the differences. Many differences between regulators are caused by their disjointed legislation, whilst others may be rooted in the different environments in which the professionals work.
Who regulates the regulators?
All nine regulators are overseen by us – the Professional Standards Authority for Health and Social Care. We are sometimes referred to as a ‘super-regulator’ or a ‘health watchdog’. We have a set of Standards called the Standards of Good Regulation. They cover the four core functions of the regulators. Every year we assess how the regulators are performing against these Standards. As part of our review we conduct audits and investigations. The result of this is an individual performance review for each regulator. We also report the results of these reviews to Parliament in one over-arching report, usually published in June.
In addition to reviewing how they are meeting the Standards, we check all of the regulators’ final fitness to practise decisions. Where we consider that the decision they reached, and the sanctions they imposed, were insufficient to protect the public, we can appeal to the courts.
We hope this whistle-stop tour around professional healthcare regulation has helped to explain, inform and educate. In part two, we look in at the role of regulation in wider healthcare at a time when there is increasing patient demand and many workforce pressures. We will also take a look at the challenges the regulators are facing and ask what alternatives are there to statutory regulation?
Related content
Watch this short video to find out more about which health and care professionals are regulated.
