by
Michael Warren, Policy Adviser
| Apr 25, 2018
What are some of the challenges for regulation?
 As we mentioned in part 1, the origins of professional healthcare regulation in the UK are mixed and varied. The oldest regulator, the General Medical Council, was founded in 1858 and healthcare provision has changed considerably in the intervening 160 years, in line with population needs and advances in medicine. This presents a variety of challenges for regulatory bodies, so let’s take a look at what they might be.
As we mentioned in part 1, the origins of professional healthcare regulation in the UK are mixed and varied. The oldest regulator, the General Medical Council, was founded in 1858 and healthcare provision has changed considerably in the intervening 160 years, in line with population needs and advances in medicine. This presents a variety of challenges for regulatory bodies, so let’s take a look at what they might be.
Legislation
Statutory professional regulation derives its powers from many different pieces of legislation. But while the bodies regulating professionals have evolved, legislation hasn’t kept up the same pace.
Not only does this affect how regulation works in practice, it also means that making changes to legislation can be complicated and slow. With regulation needing to be agile in response to extensive changes taking place in health and social care, this becomes a real problem.
Consensual disposal (one element of the fitness to practise process) is a good example of how lack of reform is constraining innovation. For anyone unfamiliar with the term, consensual disposal is a process used by some of the regulators in cases where there is agreement on the facts of the case and proposed sanctions, and where there may be no public interest or need for a hearing.
The process then has the potential to be simpler, faster and more flexible for all parties, as well as being less adversarial. So far, so good. However, not all regulators have legislation to use consensual disposal which means that those who don’t are somewhat constrained. In lieu of having these powers, those regulators are restricted to small procedural changes.
It is important to note, however, that the use of consensual disposal must be balanced with transparency and accountability. While we have the power to appeal cases which proceed to a hearing, we don’t have the same powers over consensual disposal cases. In our view, this poses a potential risk to public protection.
There are also variations between
the nine regulators due to their different legislation so collaboration, where sensible, is sometimes hindered. This variation and inconsistency stems from incremental and piecemeal changes to individual regulator's legislation. We believe what’s really needed is wide-scale reform.
Workforce pressures
‘NHS at breaking point’ and ‘Pressures on staff at unacceptable levels’.
We’re used to seeing headlines like these in the media. Workforce pressures in the NHS are a modern reality. In response, new roles are being piloted such as nursing associates who are intended to act as a bridge between the unregulated workforce and registered nurses. This will be a regulated, but not all newly introduced roles may be regulated.
So, why is this a challenge for regulation? And what is the expectation of such roles? Well, they may deliver advantages to the workforce such as flexibility and low cost. And flexibility is one important reason why statutory regulation (which tends towards inflexibility) may not be the right approach to making the best use of new roles – or relieving workforce pressures.
Teamworking
Professional regulation has always been designed to hold individuals to account. That’s fine in principle, except for the growing trend towards multidisciplinary teams in health and care systems across the UK.
In reality, many ‘incidents’ occur within teams and should be handled within the context of the team. So, there are inevitable questions being raised about how regulation can deal more effectively and efficiently with these issues. This is not aided by the divide between system regulation (regulation of places such as hospitals) and professional regulation.
Problems with the fitness to practise process
Regulators, and those who have experienced the fitness to practise process, would all agree that it can be extremely stressful for registrants and witnesses alike. This stress can be made worse in cases where it can take several years from the initial complaint to the final decision, – not an uncommon occurrence.
Decisions about cases (which may relate to the same incident or on the surface appear similar) can vary between regulators. Of course, this raises questions about the effectiveness of regulators and how fair the process really is. It can also be expensive, especially when the hearings run on for many months. So, how can fitness to practise be improved?
Without significant legislative change, there are limitations to what can be improved in the short-term which is why we will continue to push for meaningful regulatory reform. Find out more about how we think fitness to practise processes could be reformed. But there is encouraging evidence that regulators are adapting within the confines of the system. Moves are being made to modernise fitness to practise processes, such as seeking early resolution of cases and remediation where appropriate.
How are regulators adapting to meet these challenges?
Prevention is better than cure. And the regulators would agree, as they shift their focus and budgets towards the prevention of harm.
This is sometimes called ‘preventative regulation’ and can be broken down into two steps:
- Regulators collect data and insights from, and about, professionals (on what influences them) to better understand how and why harm occurs.
- Regulators use this data and share these insights with employers and other stakeholders to prevent harm from occurring.
Of course, regulation is just one factor in influencing how healthcare professionals act. So, the regulators are also collaborating with organisations which have different methods of influencing the workforce. For example, the General Medical Council has been working with NHS Education for Scotland and the Royal College of Physicians and Surgeons of Glasgow to support doctors’ professional development.
And just as multi-disciplinary teams are being adopted in clinical settings, there is also growing recognition of the value of inter-professional learning. Historically, professionals have trained and worked in silos, learning and sharing insights mainly within their own profession. But there is evidence that learning as a team creates shared values and an aligned approach to safety and quality.
Some professional regulators have adopted this thinking and changed their processes. The Health and Care Professions Council has made inter-professional education a requirement within their standards of education and training and we expect others to follow.
What are the alternatives to regulation?
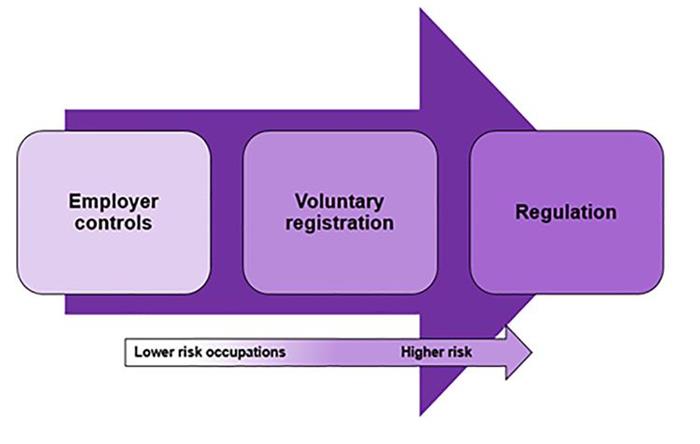
There are over 30 regulated occupations, but not all regulated occupations pose an equal risk. It may be possible for lower risk occupations to be appropriately assured by means other than statutory regulation. In fact, the recent government consultation asked the question, ‘Do you agree that the current statutorily regulated professions should be subject to a reassessment to determine the most appropriate level of statutory oversight?’
The Accredited Registers programme
There are other means of assuring that healthcare practitioners are suitable to practise. One is assured registration which is widely available to practitioners whose occupations are not governed by statute.
These practitioners can voluntarily join a register if they comply with its standards. The Authority set up the Accredited Registers programme following legislation enacted in the Health and Social Care Act 2012. Currently, 25 voluntary registers, representing 85,000 practitioners are accredited by us. This means that the organisation which holds the register has met demanding standards set by the Authority in several areas, including:
- protecting the public
- complaints handling
- governance
- setting standards for registrants
- education and training
- managing the register.
Employer checks
Employers have tools at their disposal like checking the credentials of job applicants. They should also conduct employee appraisals to assess current performance levels.
What’s crucial is that the level of assurance used to make sure someone is suitable for practice should correspond to the level of risk inherent in their practice, as shown in this diagram.
A final word…
In these two blogs, we have only just scratched the surface of professional healthcare regulation and the issues which surround it. From the outside, regulation can appear a small and uninteresting world. However, much like the Tardis, it is bigger and more complex on the inside than it might first appear.
In upcoming blogs we’ll burrow deeply into the furthest corners of regulation. In our next blog, we’ll expand on a topic which has hit the headlines recently - why does regulation need to be reformed?
Related material
Read more about this subject: