by
Denham Phipps
| May 16, 2019
No matter how many policies, procedures, processes, checklists and codes of practice are in place to assure safety and mitigate risk, in healthcare settings, there is always one unknown factor – people. In his guest blog Denham Phipps – a Lecturer at The University of Manchester and a Chartered Ergonomist and Human Factors Specialist – explains more about 'human factors' and how they can relate to practitioner regulation.
The human actor
For all of the scientific and technological advances in health and social care, its safe and effective delivery depends on the people who work within it. At their best, they bring expertise, creativity, adaptability and intuition to their work. However, the human contribution is a double-edged sword: people are also prone to becoming tired, misguided, distracted or stressed. How well health and social professionals carry out their activities, and how well they feel as a result of this work, can depend on the physical and social conditions in which it occurs.
The latter observation inspired the National Quality Board to publish The Human Factors in Healthcare Concordat in 2017. The concordat challenges healthcare organisations to examine the impact of their work settings on clinical performance. Extending this challenge to health and social care regulation raises a question: what happens when we take a human factors perspective on regulatory work?
Let’s begin by taking a brief look at practitioner risk management more broadly.
Managing risks in health and social care practice
Take a moment to consider the work that goes on within a healthcare profession. What could go wrong in this work? What could happen as a result? How would you know any of this was happening? And what could be done to prevent it?
In thinking about these questions you might imagine a pathway leading from a hazard (the potential for something to go wrong) to an undesirable event (something actually going wrong). Take for example a practitioner who should refer a client to a general practitioner, but does not. As my figure shows, this is an undesirable event brought about by a hazard such as lack of access to patient information, an inability to understand the information or act on it, or routinely disregarding patient information out of hand. Extending the pathway past the event itself, you might arrive at some consequences: the patient coming to harm; increased burden on other practitioners; a lowering of trust in the profession, distress to the practitioner involved.
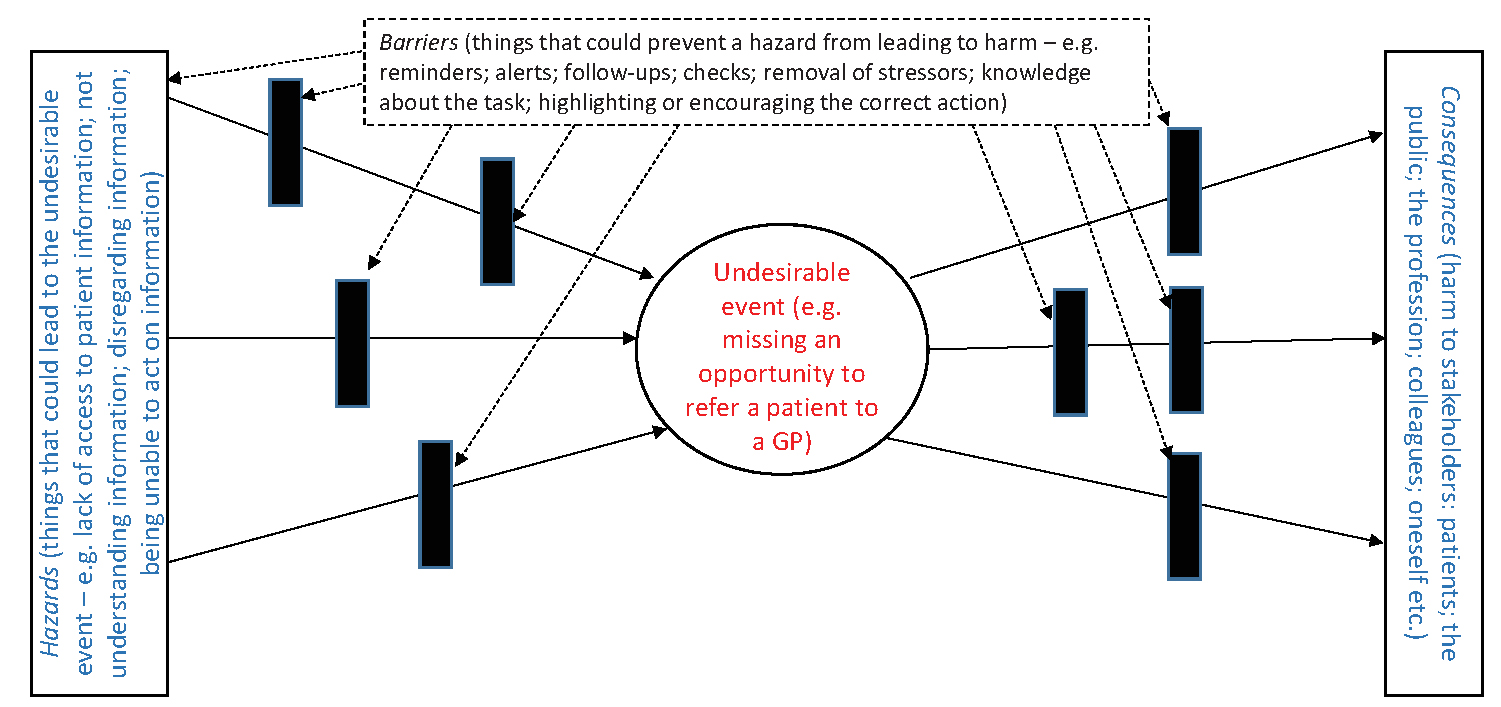
Along the pathway, though, there may arise opportunities to block the evolution of a hazard into an event, or of an event into harm. In our example, such 'barriers' could include reminders, alerts or follow-ups. Alternatively, the hazards could be addressed at source by ensuring that the practitioner has the knowledge required to undertake the task, is encouraged to carry out appropriate actions and is not unduly burdened by doing so.
This approach to understanding practitioner risk (about which you can read more here and here) places that risk in the context of the practitioner’s work system. In doing so, it leads us to a discussion about human factors.
What is 'human factors'?
In simple terms, human factors (which, incidentally, is also known as 'ergonomics', although I’ll keep to the one term here for simplicity) is the study of the relationship between people and work systems. It is based on the premise that a work system has physical, cognitive and social characteristics that influence how people within the system perform. Human factors incorporates knowledge from several scientific and technical fields – most notably physiology, psychology, and branches of engineering. However, the hallmark of human factors is its focus on the interaction between people and systems, rather than either of these in isolation.
In health and social care, a human factors approach typically looks at how the following elements come together in the course of a care activity:
- People;
- Technology and tools;
- Tasks (for example their nature and scheduling);
- The immediate environment (for example, noise, temperature and lighting);
- The organisation (for example, organisational priorities and incentives).
What could this tell us? Here is just a selection of the various insights from human factors work that are relevant to the current discussion:
- Anaesthetists and community pharmacy staff sometimes act differently to how practice guidelines or standard operating procedures suggest they should.This, though, often occurred in order to ensure that their goals are achieved given the way that their work system is operating at the time – maybe even to keep the system itself functioning;
- In the paediatric intensive care unit and the emergency department, characteristics of the work system such as workload, distractions and poor decision support have been implicated in the occurrence of prescribing errors, possibly due to the mental demand that is imposed on prescribers;
- Nurses working on a healthcare helpline have been found to change their decision-making about referring callers over the course of a shift. As the number of calls since their last rest break increases, they appear more inclined to make an urgent referral for each caller.
Having looked at what 'human factors' tells us about health and social care, we can now think about how it relates to practitioner regulation.
What are the implications for regulation?
Fitness to practise, as typically dealt with in health and social care regulation, is often framed as a matter concerning an individual practitioner – hence the focus of previous studies on personal characteristics predisposing a practitioner to performance problems. The challenge that a human factors approach poses for regulators is to reconcile this 'person-centred' view with the alternative 'system-centred' view, such that the conditions surrounding the practitioner’s work are also taken into account. In other words (and as suggested in NHS Improvement’s just culture guide) we should account for the possibility of a less than perfect work setting being implicated in a fitness to practise concern.
Two well-publicised cases illustrate this point. The first is that of Elizabeth Lee, a pharmacist who received a criminal conviction for making a dispensing error. During the shift in which this error occurred, Lee had apparently dealt with a high volume of prescriptions, possibly while fielding interruptions to her work, and had not taken a break during her 10 hours of work.
The second case is that of Dr Hadiza Bawa-Garba, who also faced prosecution after a delayed diagnosis of sepsis was implicated in the death of a hospitalised patient. In this case, Dr Bawa-Garba cited concerns about the work system, including the limited availability of staff to provide her with the support she needed and IT problems that made it difficult to gather the clinical information in a timely manner; these issues apparently making the already difficult task of diagnosing sepsis even more so.
My point here is not that health and social care practitioners – either the two mentioned here or any others – should be absolved of their professional responsibility regarding patient care. It is, though, that any scrutiny of the way in which this responsibility is discharged should include an understanding of the setting in which the practitioner is working. In other words: how much does the system help (or hinder) in doing the right thing?
So, having recognised the role of human factors in clinical performance, what should regulators do now? One recommendation is to seek human factors expertise and incorporate this into fitness to practise processes. The General Medical Council, for example, is shortly to do this, through a combination of human factors guidance during fitness to practise reviews and awareness training for investigators. Another recommendation is to incorporate human factors knowledge into the prospective work that regulators do to promote quality and safety. They could, for example, incorporate an appraisal of human factors that might affect practice in a given setting; alternatively, they could provide incentives and support for registrants to use human factors knowledge in their own quality and safety improvement programmes.
Some outstanding questions
Finally, a couple of brief thoughts about what remains to be understood about human factors and practitioner regulation. My discussion has focused on clinical performance – but where does this leave other types of issues, such as conduct and health concerns? As it happens, what is good for practitioner performance is probably also good for practitioner health, at least from a human factors perspective. In our own work on pharmacy regulation, we have explored a possible link between practitioners’ working conditions and their engagement in behaviours that could generate practice concerns of any type.
Much of what I’ve discussed here concerns doctors, nurses and pharmacists. What, though, of the various other professions that deliver health and social care, whether statutorily regulated or overseen by the Authority’s accredited registration scheme: the opticians; the podiatrists; the psychotherapists; and the clinical scientists; to name but a few? They have quite diverse roles, functions and working arrangements. For example: some professions involve solo practitioners; some are based in healthcare facilities while others work predominantly in the community; some use mainly relational rather than technical or medicinal interventions; others have a relatively limited and proceduralised scope of practice. There is a need to consider how human factors insights apply across these groups, both in terms of specific human factors issues and the strategies for addressing them.
Summary
I have given you an overview of what human factors is and how it relates to health and social care regulation. There is more to be said about this topic – and indeed, more to be yet studied – than I am able to fit into a single article. However, you now have an appreciation of why human factors matters in health and social care and what you as regulators need to know about it. I and the Authority would be pleased to hear your thoughts about the role of human factors, and what you would like to do about it.
Denham Phipps is a Lecturer at The University of Manchester and a Chartered Ergonomist and Human Factors Specialist. He can be contacted on denham.phipps@manchester.ac.uk.
Related material
The WHO defines human factors as: the study of all the factors that make it easier to do the work in the right way. A failure to apply human factors principles is a key aspect of most adverse events in health careor another definition of human factors is the study of the interrelationship between humans, the tools and equipment they use in the workplace, and the environment in which they work.